Integrating Health Services Will Improve Outcomes

As published in the San Francisco Business Times December 20th, 2019
By Brett Andrews
The United States is arguably the world’s economic leader. We are also admired globally for innovation. And we’re the consummate leader in entertainment. Yet, when it comes to health care (especially for the underserved), our outcomes are woefully inadequate.
To address this quandary, we need to take a hard look at the siloed system of health care that contributes greatly to the fragmentation of services. A person in need of medical attention may also need help with social services, substance use, aging care or mental health. Due to its complexity, this separation leads to many people falling out of care.
Simply stated, fragmentation of health care services doesn’t work.
In 1948, the World Health Organization boldly said that, “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” Over the past 70 years, countries around the world have worked to develop a variety of health care systems based on this model – some with great success. This brings me to our own country. For decades, a medically focused paradox has existed within the U.S. health care system. While Americans spends substantially more money on health care than any other industrialized nation, why do we have such relatively mediocre health outcomes? The comparison is most striking when compared with Scandinavian countries. They spend considerably less on both health care per capita and as a percentage of GDP, yet they achieve substantially better health outcomes than we do.
What does all of this mean on a local level and how can integrated services address some of our most pressing societal challenges? Let’s start by looking at the health of our street population. Homelessness continues to be a growing problem in San Francisco. Despite spending approximately $300 million annually on homelessness, service outcomes for San Francisco’s homeless population have remained relatively unchanged over the past decade. Earlier this year, a homeless census survey called a Point-in-Time Count revealed even more extreme numbers and statistics. The number of unhoused individuals increased by nearly 1,000 to approximately 8,000. Given these historic outcomes, it’s hard to deny the correlation, if not causation, of a fragmented system of care and less than ideal health and economic outcomes in our community. A deep look into San Francisco’s service delivery model reveals a strong foundation of services and robust data about our marginalized population, but also a siloed and uncoordinated system of care structure with limited capacity to share information.
So what are we to do? And where do we start?
Due to expanded health care provided through the Affordable Care Act, many local systems of care and health and human services nonprofits across the country have needed to restructure, with a priority focus on integration. Strong empirical evidence suggests that physical health outcomes can be improved by integrating social services such as aging care, housing assistance, mental health and substance use treatment, benefits and health care counseling, nutrition programs, employment services and emergency financial assistance. San Francisco has taken up the charge of assessing its system of care, with an eye toward integration. Recent efforts like the Whole Person Care Initiative, the hiring of San Francisco’s Behavioral Health Reform director and Mental Health SF are good examples of emerging and innovative public health and community-based partnerships that aim to serve the complete person.
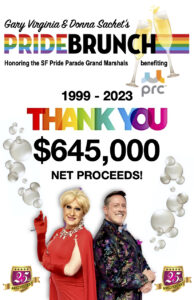
PRC, where I work, recently completed a double merger acquiring Baker Places, a mental health and substance use disorder residential treatment agency, and AIDS Emergency Fund, an emergency financial assistance agency. Valuing the effectiveness and efficiency of integrated services, PRC consolidated the three organizations and designed a framework that supported the de-siloing of multiple funding sources. We also integrated fragmented services into a continuum of treatment and social services – bringing everything “under one roof” and placing clients’ perspectives at the center of our organization. PRC has learned how to design an integrated model of care that moves more than 5,400 unstably housed individuals, struggling with mental health and addiction, from crisis to stabilization. With 267 treatment and supportive housing beds, in concert with wraparound support services that give people all necessary tools and support, we’re helping to reshape and reclaim their destiny.
Through it all, what remains abundantly clear is this: The abiding commitment and resolve we all share in our desire to tackle these social issues. These challenges impact not only those most vulnerable, but also those who desperately want to help, and just want to know how. We have a history of success on our side – let’s celebrate and build on it.